Table of Content
We hope that the above set of questions will support efforts to refine our approach to quality indicators, to focus on the overall objectives rather than the individual indicators and to measure what really matters to patients, professionals and policymakers. In other words, equity and patient-centeredness were traded off in favour of safety and efficiency. We can see from this example that sets of quality indicators can never be a neutral assessment of care, but must always be considered from a particular vantage point of patients, clinicians, insurers or other parties. It will remain important to ensure that dropping the indicator does not result in this becoming a problem again, using alternative methods such as inspection visits or taking samples, rather than continuous measurement through quality indicators in all facilities.
When she’s not researching the most effective employee management techniques, Andjelka loves cooking, reading, and fighting for human rights. Tracking this number will give you an insight into your employees’ job satisfaction, how successful you are at retaining caregivers and whether your agency is more or less effective when compared to the industry as a whole. Caregiver turnover is the percentage of caregivers that left your agency within a given time frame. To calculate this KPI, divide the number of caregivers left by the number of all caregivers that worked during a given time. You can determine your agency's profit margin ratio by deducting total expenses from total revenue and dividing this sum by total costs. Track this KPI to identify profit drivers - internal and external factors that affect your business's profit.
Financial KPIs
The objective was to conduct a systematic review of toolkit evaluations intended to spread interventions to improve healthcare quality. We aimed to determine the components, uptake, and effectiveness of publicly available toolkits. Besides financial profit drivers, such as price or service volume, non-financial profit drivers are also significant to consider. They include customer satisfaction, productivity, service quality, employee satisfaction, etc. Some of these drivers are mentioned above and below, as key performance indicators for home health care.

Technical documentation for calculating process measures can be accessed via the link to Technical Documentation of OASIS-Based Measures in theDownloadssection below. New Jersey is home to over 2,000 licensed hospitals, nursing homes, and medical care facilities. The New Jersey Department of Health works to ensure that citizens receive appropriate levels of care in every regulated facility.
Patient consent for publication
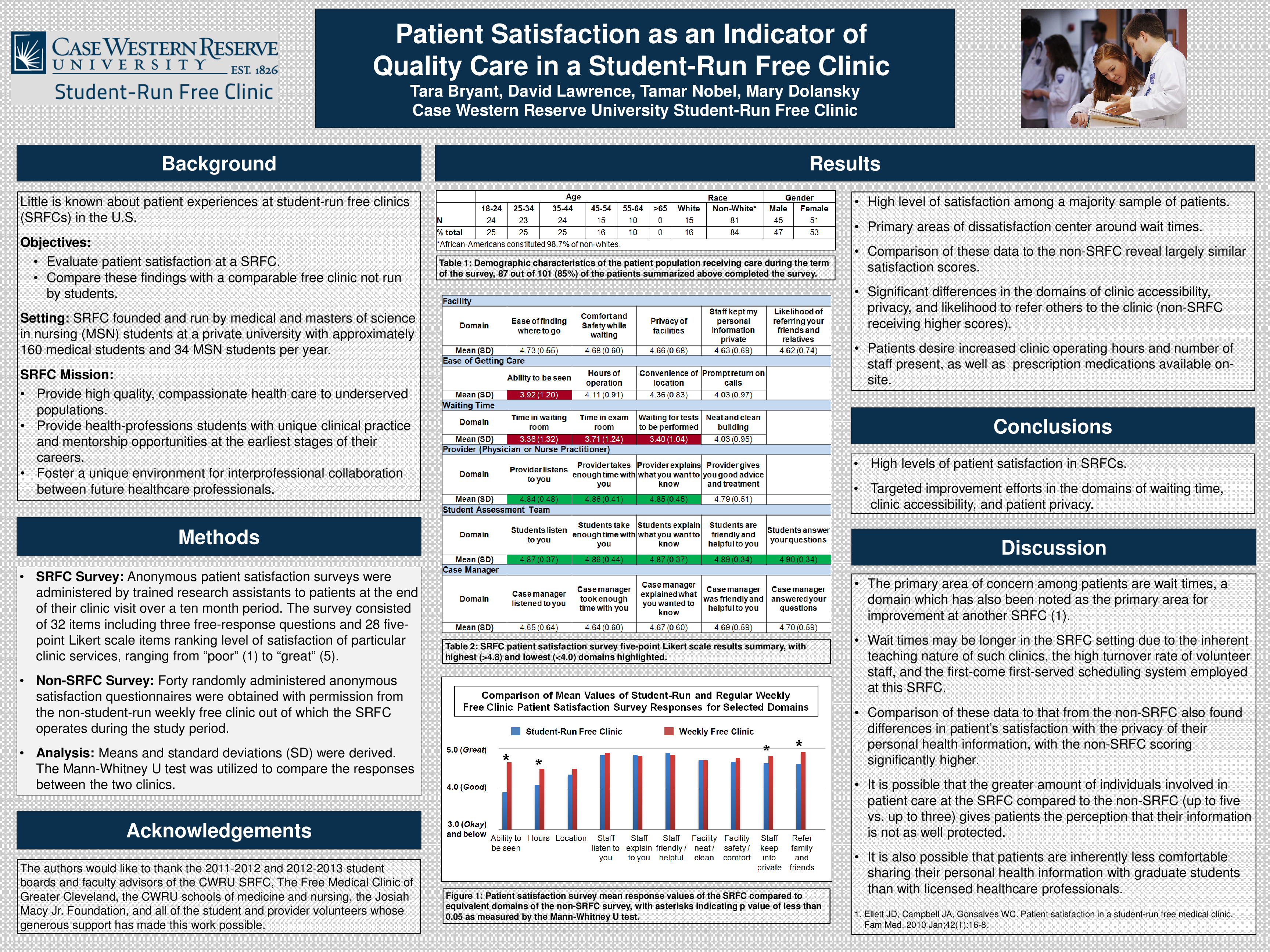
This study was a cross-sectional mixed-methods analysis of in-depth multimodal data from 31 POs affiliated with 22 purposefully selected health systems in 4 states. This study offers a provisional framework that can help in structuring thinking, policy and practice. By outlining the range of domains relevant to remote antenatal care, this framework is likely to be of value in guiding policy, practice and research. The objective of this paper is to review evidence on survey administration strategies to improve response rates and representativeness of patient surveys. Exploring how often inquiries turn into admissions will help you answer various questions.
A set of standards can help identify providers who serve veterans and deliver high-quality care. Such analysis can help you determine whether there is anything in the process that makes the prospective clients give up using your agency's services. By tracking KPIs for your primary goals, you will know if your team is reaching home health productivity benchmarks, and you can implement incentives based on their achievements.
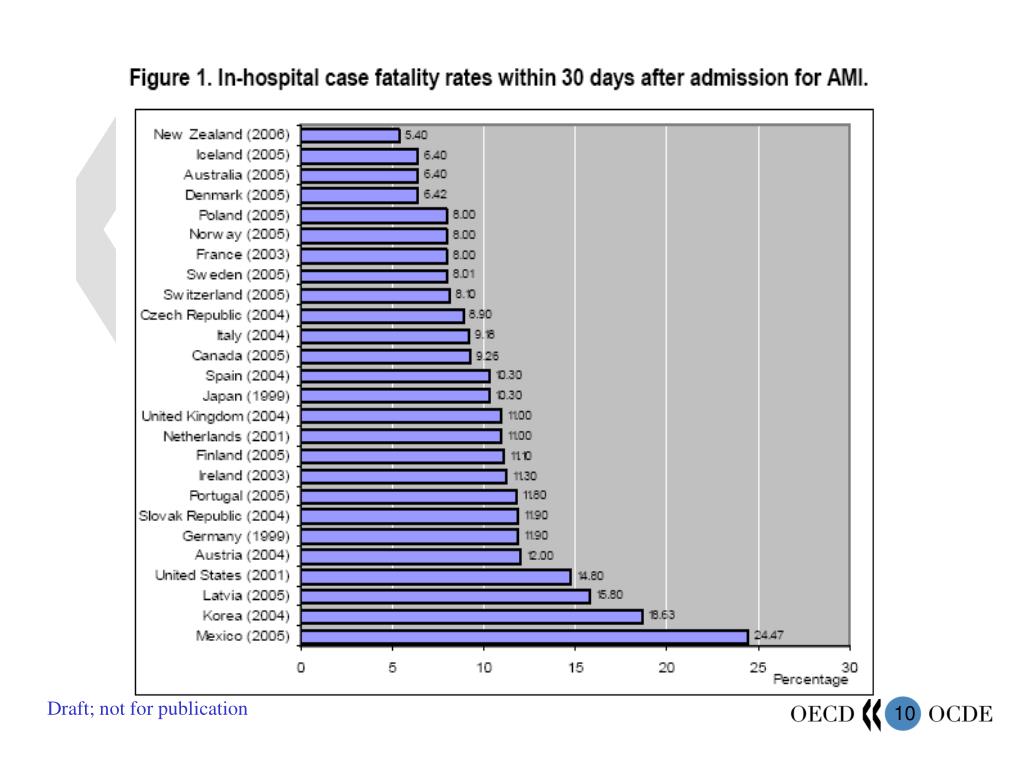
Health Care Quality Indicators
The Health Care Quality and Outcomes programme previous known as Health Care Quality Indicators Project was initiated in 2001. The aim was to develop and report indicators for international comparisons of health care quality. Over the past twenty years, data collection and analysis have been carried out, progressively expanding the coverage of the dimensions within the framework above and the number of countries involved. Prevention Quality Indicators identify "ambulatory care sensitive conditions", which are conditions that can be effectively treated in an outpatient setting, potentially preventing the need for inpatient hospital admissions. PQIs can be used as a "screening tool" to flag potential health care problem areas and provide possible insight in to the sufficiency of primary care access or outpatient services in a community, help public health agencies. That's why it's crucial to pay attention to all the warning signs that may point to their dissatisfaction with their job or that may lead to caregiver burnout.

As home health quality measures reports are public, they can compare the results with other providers. HH QRP measures derive from three data sources, Outcome and Assessment Information Set assessment, Medicare fee-for-service claims, and the Consumer Assessment of Healthcare Providers and Systems (CAHPS®) Home Health Care Survey. OASIS and HH CAHPS data collection and reporting are requirements for providers participating in the HH QRP. Medicare FFS claims data are submitted by HHAs to receive payment for services provided for Medicare FFS patients. The project focused on existing services provided in the Commonwealth Home Support Programme and Home Care Packages Program.
Using CAHPS Patient Experience Data for Patient-Centered Medical Home Transformation
The data collected by tracking KPIs provides statistics and enables a home healthcare agency to analyze its progress over a specific time, compare it to its industry peers and look for ways to improve its performance. The National Quality Forum , a multistakeholder organization established to standardize health care quality measurement and reporting, has endorsed several consensus standards for skilled home health services. Process measures evaluate the rate of home health agency use of specific evidence-based processes of care. The HH process measures focus on high-risk, high-volume, problem-prone areas for home health care. These include measures pertaining to all or most home care patients, such as timeliness of home care admission.
HCQA applies these Quality Indicator tools to the New Jersey inpatient discharge data to come up with data that measure healthcare quality. The data help hospital administrators and DOH to identify potential areas of concern that may need further investigation. Increasingly, tools and surveys are employed to determine current and optimal levels of health care service and performance, and ultimately to improve the levels for each. RAND helps policymakers, health care leaders, and practitioners determine cost-effective and accurate ways to measure the quality of health care being provided, and then recommends ways to improve the level of health care quality. KPIs need to address all aspects of a business, from the quality of care and client conversion to HR, marketing, and finance.
The number of quality indicators has proliferated, without a parallel emphasis on understanding the relationships between indicators or their contribution to the overall objective of monitoring one or more aspects of the quality of care. Instead, the number of quality indicators has increasingly become a burden, rather than a useful tool to help us achieve safer and better care. We argue that a focus on the construct being measured and assessing the validity of a set of indicators is needed to achieve that aim. This is a very different approach from simply creating more and more indicators covering every aspect of care and hoping that they will collectively amount to a useful measure of quality. When designing a questionnaire or developing a psychological test, we are careful not to overburden respondents and therefore measure only what matters to assess the underlying construct and meet the objectives of the study or programme.
Percentage of patients reporting that home health providers treated them as gently as possible. The development of measures for home health is in the early stages, but several measures have been endorsed by NQF and are being reported. Here are some examples of measures that would be appropriate for reporting to consumers and are currently included in the Centers for Medicare & Medicaid Services’ (CMS’) Home Health Compare Web site. The Patient Safety Indicators provide information on potential in hospital complications and adverse events following surgeries, procedures, and childbirth. PSIs can be used to help hospitals identify potential adverse events and assess the incidence of adverse events and in hospital complications. On February 7, 2022, the RAND Corporation convened a Technical Expert Panel web meeting to gather input about the potential development of a measure to capture value-based care arrangements Medicare Advantage organizations have with their contracted providers.

No comments:
Post a Comment